Do you ever wonder if your stress, anxiety and IBS symptoms are somehow all connected? Have you ever noticed how your anxiety levels start to rise when you have an IBS flare up… which then leads to more anxiety… which leads to more pain and gut issues? And how the more stressed and worried you become… your stomach symptoms feel like they’re never going to go away?
Well if you’ve found yourself wondering about this vicious IBS and anxiety cycle, then this post will help you to make sense of it. And most importantly let you know how you can break this very cycle.
So let’s dive in!
When it comes to IBS, stomach problems, stress and anxiety they can form a really tight cycle. And unfortunately overtime this cycle can become more and more automatic, until you start to question which came first – the stomach problem or the stress and anxiety?
Let me give you an example of what I mean.
So let’s say Toby started to develop IBS symptoms after a bout of gastroenteritis. This upset to his digestive system lead to ongoing changes in his bowel causing pain, gas and alternating constipation and diarrohea. Toby started to get worried. Why wasn’t his stomach getting any better? And all of these gut symptoms started to impact his daily routine, his eating habits, and he started to worry about the impact on his health, his work, his relationships and social life. It started to impact his sleep, and his symptoms started to get more and more frequent. What was wrong with him?!
IBS symptoms can fire up your stress response
Now all of this worry and stress fired up his bodies stress response. This happens when your body registers stress and includes a predictable chain of physical events, as your brain releases stress hormones and prepares your body for ‘fight’ or ‘flight.
When this happens your heart rate speeds up to supply blood to your large muscle groups such as your legs, your breathing gets faster to increase oxygen supply, and your liver releases glucose to provide fuel to your muscles. Your blood supply is also diverted AWAY from your gut and TOWARDS your large muscles to enable your body to either stand and fight or take flight and run away!
These automatic physical changes can cause radical changes in the activity of your gut, for example increasing muscle spasms (which can feel incredibly painful) or even shutting down all motion, resulting in diarrhoea or constipation, or alternating bouts of all three.
What’s more, the sensitivity of your gut also increases, making you all the more aware of how your gut is functioning. And when this happens, symptoms like nausea, acid reflux, abdominal pain, bloating, and excess wind become common.
Psychological stress is just as much as a trigger as physical stress.
The problem in today’s world is that this automatic response to stress can turn on when you don’t really need it to, and there is no physical emergency or mountain lion to escape from. For example worrying about your IBS and stomach problems, feeling overwhelmed about what’s happening to your health, and worrying about whether you’ll ever get your gut issues resolved. Psychological stress is just as much as a trigger as physical stress.
So in Toby’s case, all his worries, the anxiety and stress he’s feeling about his stomach problems is actually firing up and keeping his body in a constant state of stress. Which is having a significant impact upon this digestive system.
This is because your gut and your brain are inextricably connected, meaning what happens in your head can affect your gut, and what’s happening inside of your gut can affect whats hapoening in your head. And can make anxiety a lot worse. You can learn more about the gut-brain connection and it’s role in IBS in this post: Is a Faulty Gut Brain Connection Causing Your IBS?
So back to Toby.
His ongoing worry and anxiety over his IBS and stomach problems is now triggering further bowel issues… which is disrupting his social life and daily life even more. Which is creating more stress and anxiety… and so the cycle repeats.
Breaking the Anxiety and IBS Cycle
So now you know about this vicious cycle, how do you break it?
Well you first need to understand the 3 main factors which are maintaining and it. And these are:
- Firstly overall life stress. And this can come from any area of your life – from your career, finances, relationships, family… and is one of the most well-known factors responsible for symptom flareups.
- Secondly, the thoughts and beliefs you specifically have about your IBS. This includes continuously thinking about the same upsetting or anxious thoughts, assuming the worst about your IBS symptoms, feeling completely out of control and believing that things will never change.
Thoughts have a powerful effect on the body, and one of the first tasks I get my clients to do is to start becoming more aware of their thoughts. By becoming aware of what’s happening inside of their head they can learn to change their thoughts into healthier and more helpful ways of thinking… which in turn will change the way they feel.
- And lastly, the coping behaviours that you ”do” with your IBS. Another name for these behaviours is safety seeking or avoidance behaviours – these are the things you do that while they may make you feel better in the short term, are actually stealing the joy from your life in the long term. Not only that, these behaviours are actually triggering your bodies stress response, and in turn gut symptoms, because your body believes that there is a threat – and therefore reacts to it.
Types of coping behaviours include being hypervigilant, or hyper aware of your symptoms, avoiding going out or making sure there is a toilet close by, checking your bowel movements every time you go to the toilet, taking medication ‘just in case’, and only going out when you know the toilet access and there may be less people about.
Physical and emotional stress can trigger your IBS symptoms
So the outtake here is I hope really clear. Not only are your gut and brain connected, but physical, social and emotional stressors including your thoughts and beliefs can all result and trigger your IBS symptoms – because of the impact stress has on your gut.
So to break the cycle, the aim isn’t to identify the cause of your symptoms (because trust me, you can get really caught up in this!), but rather to focus on the solution.
And that is learning how to switch off your stress response, also known as your Sympathetic Nervous System. And instead switch on your rest and digest mode – activating the Parasympathetic nervous System. In this state, the stress symptom cycle is stopped, blood flow is restored to your gut, pain is reduced and gut motility is normalised. This allows digestion to start up again.
So how do you switch on your rest and digest mode?
Well in addition to reducing the impact of the 3 factors I mentioned above which are maintaining your IBS symptoms using cognitive behavioural therapy, you can also use hypnosis to gently guide your body into relaxation – giving your nervous system a well deserved rest.
This is why CBT and hypnosis are such an effective combination for getting long term relief from IBS.
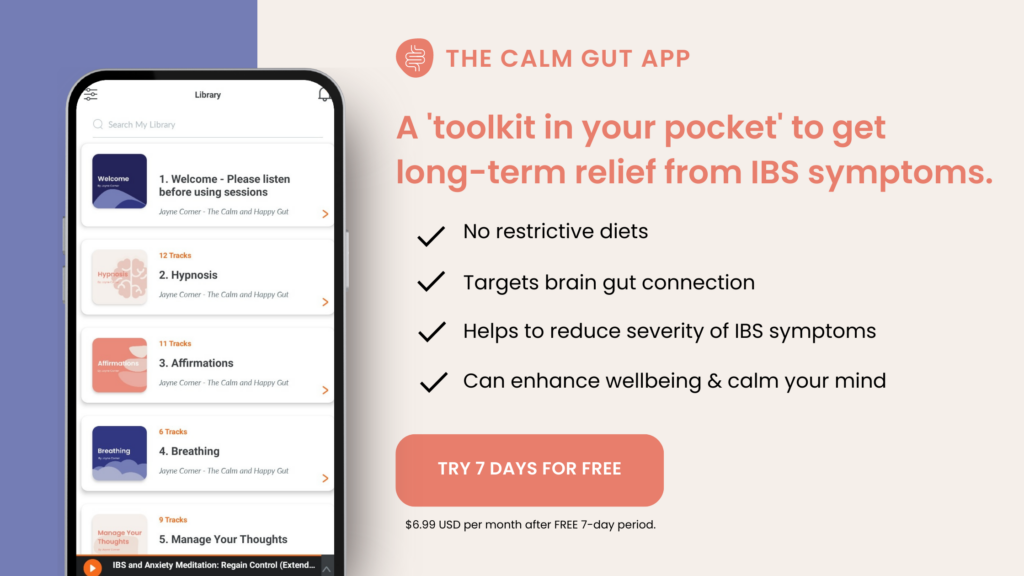
If you would like to experience what hypnosis feels like for IBS and start reducing the stress inside of your body then you can access a FREE 7 Day Trial to The Calm Gut App. This is an evidence-based audio ‘toolkit’ to help reduce the symptoms of IBS and ‘fix’ the miscommunication between your brain and your gut. Access gut directed hypnotherapy, Cognitive Behavioural Therapy (CBT), mindfulness techniques & breathing exercises at your fingertips.